Abstract
Natural killer (NK) cells are an emerging cellular immunotherapy for patients with acute myeloid leukemia (AML); however, the best approach to maximize NK cell anti-leukemia potential is unclear. Paradigm-shifting reports have shown that NK cells exhibit "memory-like" properties following hapten exposure, virus infection, or combined cytokine pre-activation. We and others have established that human cytokine-induced memory-like NK cells display enhanced re-stimulation responses to numerous activating stimuli, including tumor target cells. We have translated this finding into a potential cellular therapy for rel/ref AML patients, and have completed the dose escalation of a phase 1/2 study. We demonstrated that donor memory-like NK cells expand in patients' blood and bone marrow and retain enhanced functionality ex vivo. Further, of the 11 evaluable AML patients, we have observed 7 clinical responses, including 6 patients with CR/CRi. Since NK cell recognition depends on signals from multiple activating and inhibitory receptors, we developed mass cytometry panels to immunophenotype and track the diversity and effector functions of these human in vivo-differentiated memory-like NK cells.
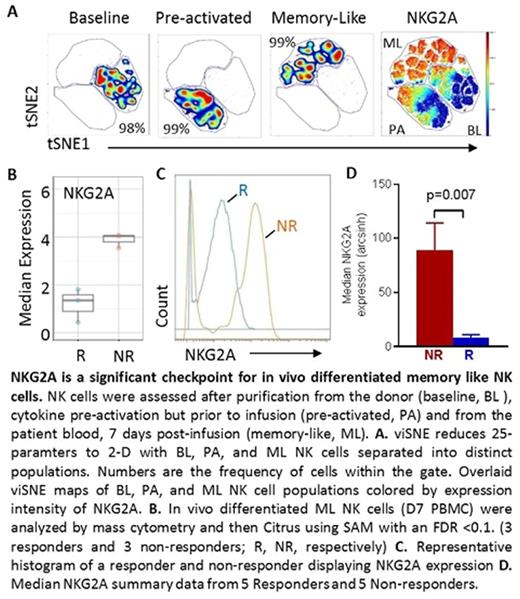
Mass cytometry revealed that in vivo-differentiated memory-like (ML) NK cells were distinct from baseline (BL) NK cells from the same donor, as well as NK cells from normal donor PBMC. Multidimensional analyses revealed a memory-like phenotype: CD56hi CD11blo CD62L+ NKG2Ahi NKp30hi Ki-67+ (baseline: 2.7% ± 0.45% v memory-like: 87.4% ± 5.3%, mean ± SEM within memory-like gate). Furthermore, Citrus analyses revealed that higher NKG2A expression was significantly correlated with treatment failure [TF median NKG2A= 89.2 ± 25.0; responder median NKG2A= 8.1 ± 2.9 (mean ± SEM); p = 0.007, n = 5 each group; SAM FDR <0.1]. NKG2A is a C-type lectin receptor with two immunoreceptor tyrosine-based inhibitory motifs. Signaling through NKG2A is achieved when it engages its ligand, HLA-E. HLA-E is a non-classical major histocompatibility complex class I molecule that is expressed abundantly on many normal tissue types as well as tumors, including AML. Based on these findings that NKG2A is upregulated on memory-like NK cells and the intensity of NKG2A on memory-like NK cells correlates with patient responses, we hypothesized that NKG2A/HLA-E interactions in vivo represent a major barrier to memory-like NK cell responses.
In order to interrogate the role NKG2A may play in limiting cytokine-induced memory-like NK cell responses, we stimulated in vitro-differentiated ML cells with the K562 AML tumor line displaying forced expression of HLA-E (K562-E) in the presence of isotype or anti-NKG2A blocking antibody. Increased IFN-γ (p = 0.02) and TNF (p = 0.05) production by NKG2A-blocked ML NK cells was detected, compared to isotype-treated ML NK cells. We performed a similar stimulation assay using primary AML blasts as targets, which express a variable level of HLA-E. Again, ML NK cells treated with NKG2A blockade produced significantly more IFN-γ than isotype-treated ML NK cells (p = 0.001). Studies examining NKG2A checkpoint blockade on in vivo-differentiated ML NK cells from AML patients are ongoing. In conclusion, in vivo-differentiated cytokine-induced memory-like NK cells are phenotypically distinct from conventional NK cells. Further, targeting NKG2A expressed on ML NK cells in vivo has the potential to enhance the clinical efficacy of memory-like NK cell therapy for patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.